OMC at a Crossroads: What’s Broken, What’s Fixable, and What Comes Next
Olympic Medical Center is facing a financial and operational crisis—but a data-driven turnaround is underway, and the choices we make now will shape access to care and jobs across Clallam County.
Editor’s Note
The following article was developed primarily from the substantial research and writings of Steven Pelayo, whose detailed analyses and community discussions have helped illuminate the challenges and opportunities facing Olympic Medical Center. His work—shared across public forums, community groups, and with the Port Angeles City Council—provides the foundation for nearly every insight contained here.
Clallam County Solutions’ role has been to compile Steven’s thoughtful contributions, add relevant context from public meetings and reports, and present this as a single, comprehensive story. Our goal is to honor the depth of Steven’s work, highlight his reasoned approach, and make this important conversation accessible to the broader community.
Why OMC Matters Right Now
Olympic Medical Center is more than a building—it’s the backbone of care on the North Olympic Peninsula and one of Clallam County’s largest employers. When OMC is healthy, families get timely care close to home, jobs are stable, and local dollars keep circulating. When it falters, we all feel it: longer waits, deferred services, and stress on hundreds of livelihoods tied to the hospital’s payroll and purchasing.
The current crisis is visible in everyday life—MRIs that take months, specialists leaving, and staff stretched thin. The key, though, isn’t to wallow in what’s wrong; it’s to own what’s fixable and act. That means doing two things at once: (1) facing facts about financial losses and self-inflicted setbacks (like compliance lapses and the 340B miss) and (2) executing local, practical improvements—better scheduling and throughput, accurate documentation and revenue capture, clear access metrics, and transparent reporting the public can follow.
Clallam County Solutions exists for this kind of moment. We’ll credit what’s working, name what isn’t, and keep the focus on solutions that protect patient care and local jobs. OMC’s future isn’t a partisan question; it’s a community project. With disciplined execution and steady governance, we can preserve high-quality local care and the economic stability it supports.
The Numbers: What the Crisis Looks Like
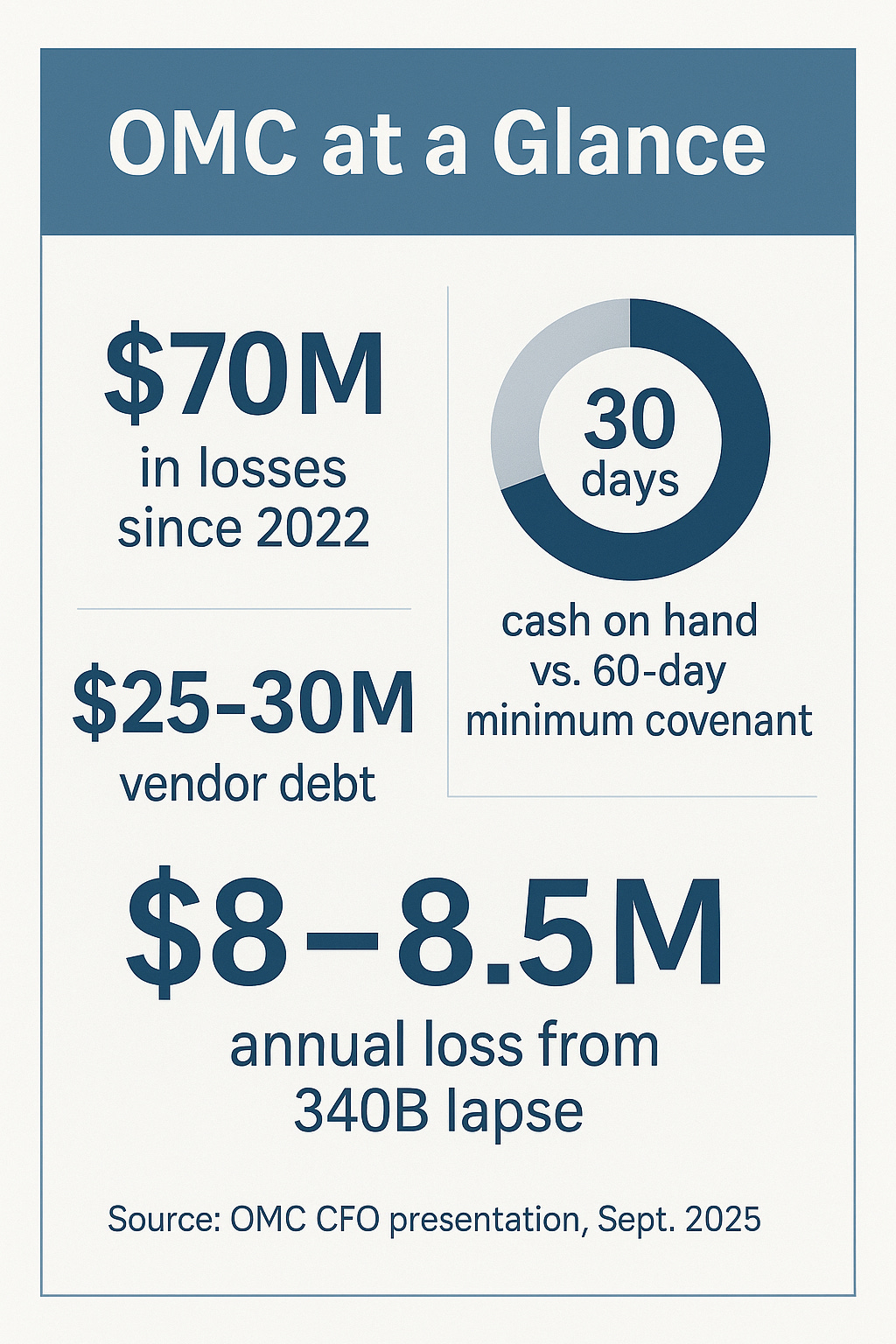
Olympic Medical Center’s challenges are not abstract—they’re measurable, and they’re serious. “According to OMC’s September 2025 Interim CFO presentation, the hospital has lost roughly $70 million since 2022 and now carries about $25–30 million in unpaid vendor bills. As of this fall, the hospital has about 30 days of cash on hand, well below the 60-day minimum required under its loan covenant with KeyBank—a technical breach that limits flexibility and heightens financial risk.
But cash shortfalls only tell part of the story. About 85 percent of OMC’s patients rely on Medicare or Medicaid, programs that reimburse below the cost of care. That’s a national challenge for rural hospitals, but OMC’s current situation also reflects a series of local management failures that magnified those pressures.
One of the biggest: the loss of the federal 340B drug-pricing program, which had saved the hospital an estimated $8–8.5 million annually. The program wasn’t “suspended” by Washington—it was lost because of internal missteps in compliance tracking. As Pelayo notes, “There are entire consulting firms built to make sure hospitals maintain eligibility. We took our eye off the ball.” Combined with earlier compliance issues involving CMS and DOH, these are mistakes that could have been avoided—and each one has real financial consequences.
OMC’s interim CFO, Dennis Stillman, has also flagged vendor payments as a mounting concern. Payables should ideally sit in the “mid-teens” of days outstanding, but they’re now nearly double that. This is more than an accounting issue—it affects local contractors, suppliers, and partners who rely on timely payment.
Meanwhile, revenues aren’t keeping pace with costs. “We can’t cut our way to prosperity,” Steven Pelayo reminds us. “At some point, we have to grow.” Growth means improved utilization—seeing more patients, retaining more procedures locally, and using the staff and facilities we already have more effectively.
The bottom line: OMC faces a financial crisis, but not an irreversible one. Its current cash position and payables are warning lights, not a death sentence. What happens next depends on whether the community can sustain the discipline, transparency, and urgency needed to rebuild both trust and solvency.
Causes: Two Halves of the Same Story
It’s easy to blame Washington, D.C. for OMC’s struggles—and yes, rural reimbursement formulas are stacked against small communities like ours. But as Pelayo emphasizes, the harder truth is that much of OMC’s crisis is self-inflicted. The financial damage we’re facing didn’t come solely from national policy; it came from local oversight failures and missed accountability that allowed preventable problems to compound.
Part One: Self-Inflicted Headwinds
Over the past several years, OMC has weathered three major setbacks that were largely avoidable:
CMS and DOH compliance violations, which required outside consultants to fix and temporarily jeopardized reimbursements.
The loss of the federal 340B drug-pricing program, which had provided $8–8.5 million in annual savings and was forfeited through internal process failures, not regulatory bias.
Chronic underperformance in revenue management and scheduling systems, which left productivity and billing opportunities on the table.
Each of these was, in Pelayo’s words, a “major screw-up.” They were not the inevitable result of federal underpayment—they were operational failures that reflect years of complacency. “We took our eye off the ball,” Pelayo says, “and the community deserves an honest accounting of that.”
The 340B lapse alone is enough to illustrate the cost of inattention. Hospitals across the country employ full-time teams or specialized consultants to ensure eligibility doesn’t lapse. OMC did not. The resulting loss of $8–8.5 million per year is money that could have paid vendors, retained staff, or reinvested in equipment—and because requalification can take up to two years, the impact will stretch well into 2026.
Part Two: Structural Pressures
That said, OMC also operates within a national system that makes stability difficult. As mentioned, roughly 85 percent of its patients are covered by Medicare or Medicaid, which reimburse below the cost of care. Inflation in labor and supply costs, combined with the ongoing shortage of nurses and specialists, leaves hospitals like OMC with thin margins even in good years.
But those realities don’t excuse what happened locally—they make local discipline even more important. The federal model won’t change overnight. What OMC can control is execution: compliance, scheduling, billing accuracy, and financial oversight.
As Pelayo puts it, “We have to own what we can fix.” That means acknowledging mismanagement where it occurred, learning from it, and refusing to repeat it. The way forward starts with honest self-assessment—because a hospital can’t rebuild credibility without first confronting its own role in the crisis.
Turning the Ship: What Management Is Doing Now
For the first time in years, Olympic Medical Center is confronting its problems directly. Under the interim leadership of CEO Mark Gregson and Interim CFO Dennis Stillman, the hospital is rebuilding credibility by grounding every decision in data, transparency, and measurable results.
A Culture of Accountability
Gregson and Stillman have implemented a new performance dashboard that tracks key indicators—cash on hand, vendor payables, provider productivity, infection rates, patient throughput, and staff engagement. These metrics are now reviewed regularly by the board and management in open meetings. Gregson has emphasized that the numbers will be shared “for better or for worse,” signaling a shift toward honesty over comfort.
At the same time, the leadership team is tackling the inefficiencies that have long held OMC back: outdated scheduling, poor data flow between departments, and underutilization of staff. Aligning daily operations with patient demand could generate as much as $1 million per month in savings and new revenue opportunities—without layoffs—simply by right-sizing staffing and improving throughput.
Investing in Expertise
OMC’s engagement with the consulting firm Chartis—openly discussed at board meetings—has drawn both criticism and praise. The firm was brought in to help OMC resolve its CMS and DOH compliance issues and strengthen operational controls. With OMC’s annual revenue near $330 million, the consulting expense represents a small fraction of total operations.
As Pelayo notes, the point isn’t how much it costs, but what it delivers. One identified right-sizing initiative—once implemented—will more than cover the combined cost of interim leadership and consulting services. “His pay is irrelevant,” Pelayo says of Gregson. “His expertise is essential. If we’d hired him two years ago, we’d have lost significantly less money.”
Pelayo also points out that Gregson’s role is both necessary and thankless. “He’ll end up being the fall guy,” Pelayo says, “because change means cuts, and cuts create tension. But that’s exactly why a turnaround specialist was needed now—so a future permanent CEO can start fresh.”
Rebuilding Systems and Trust
Beyond financial repair, OMC’s new leadership is prioritizing cultural renewal. Employee town halls, engagement tracking, and new feedback mechanisms are designed to rebuild trust internally. Staff are encouraged to share ideas for improvement, knowing they’ll be heard rather than dismissed.
Gregson’s team is also restoring credibility externally by increasing transparency with the community. The goal is not to hide the pain of change but to demonstrate that change is purposeful. Each improvement, each metric, and each cost reduction ties back to one idea: keeping local healthcare viable.
As Pelayo summarizes, “Turnarounds aren’t easy—but the cost of doing nothing is worse. The hospital is finally being run with accountability, and that’s something the community should want to see through.”
The UW Option: Partnership Without a “White Knight”
As Olympic Medical Center stabilizes its operations, one topic continues to spark both optimism and confusion: a potential affiliation with UW Medicine. The idea of linking with one of the Pacific Northwest’s most respected medical systems is compelling—and rightly so. UW brings scale, expertise, and credibility that few rural hospitals can achieve alone.
But as Interim CEO Mark Gregson and Pelayo have both emphasized, this partnership—if it moves forward—will not be a financial rescue. The two organizations signed a non-binding Letter of Intent in mid-2025 to explore potential collaboration models. The process is still early, with months of due diligence ahead and no commitment to funding, acquisition, or debt relief.
What UW can offer, however, is capacity and leverage. A partnership could strengthen specialty care, expand access to telemedicine, and provide a platform for clinical collaboration and shared technology. It could also improve OMC’s ability to recruit and retain physicians, who are increasingly drawn to systems with academic and research ties.
Beyond operations, UW’s scale matters for another reason: advocacy. Rural reimbursement reform depends on bipartisan engagement in Washington, D.C.—and historically, OMC has lacked that reach. As Pelayo points out, “We need to partner with someone who can help us build bipartisan support. For too long, our representation in D.C. has leaned one-sided. UW has the connections and credibility to give our community a stronger voice on both sides of the aisle.”
That political and policy influence could prove as valuable as clinical collaboration. In a federal system where Medicare and Medicaid rules drive rural hospital solvency, being part of a respected statewide network amplifies OMC’s ability to be heard.
Still, no partnership will succeed if OMC enters it from a position of instability. UW is unlikely to formalize an agreement with a hospital still in financial crisis or local turmoil. “More disruption now,” Pelayo warns, “could jeopardize those talks entirely.” The current turnaround—however uncomfortable—is the foundation on which any future affiliation must be built.
In short, the UW partnership is not a white knight, but it could be a force multiplier. It won’t erase OMC’s financial problems, but it can amplify its strengths—expanding care options, improving advocacy, and securing a seat at the table in the broader healthcare policy conversation. The first step, though, remains ours: get stable, stay disciplined, and earn the kind of partnership that strengthens—not replaces—local control.
The Hard Fork Everyone Whispers About: Critical Access
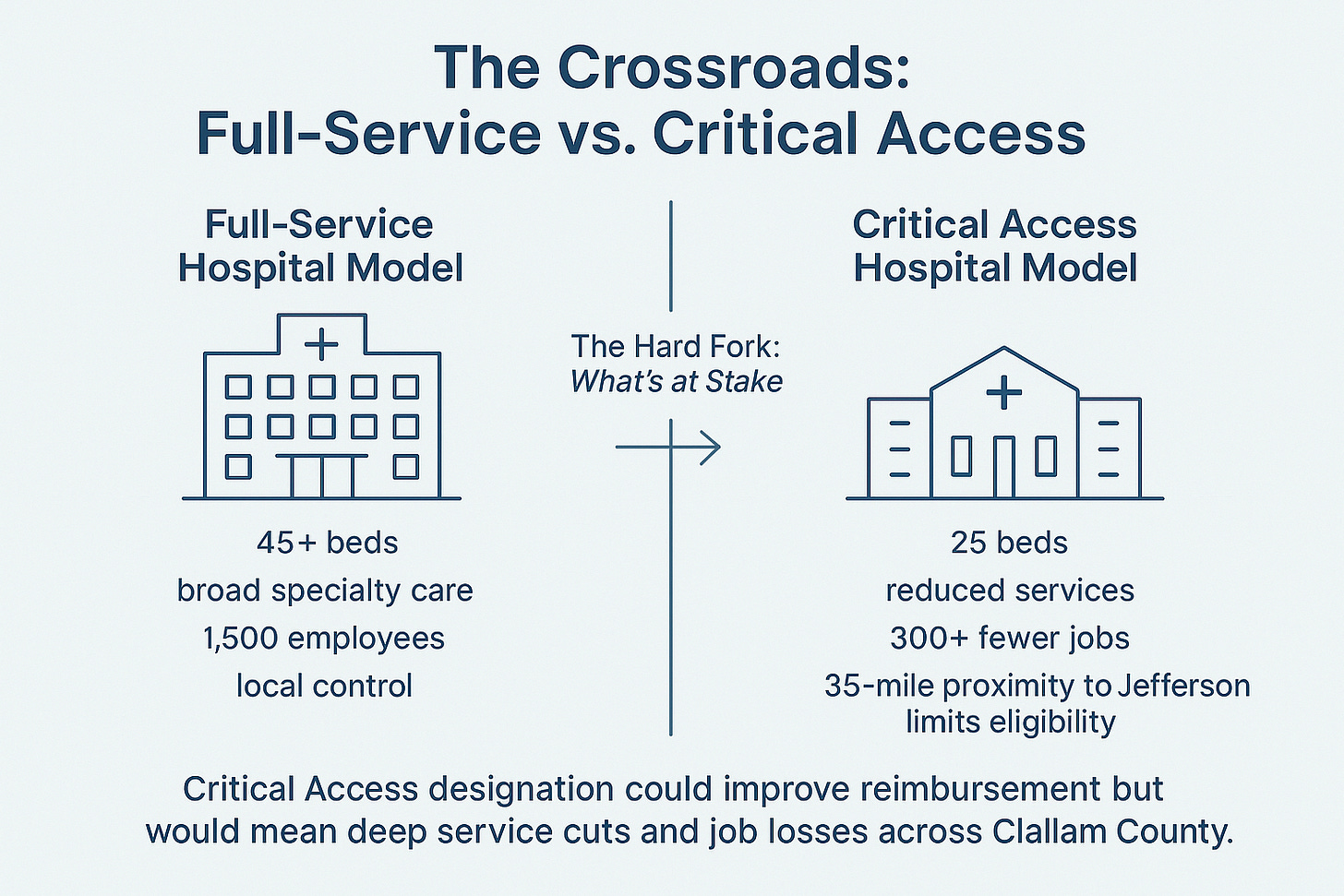
Behind closed doors—and increasingly, in public discussions—a difficult question keeps resurfacing: should Olympic Medical Center consider converting to a Critical Access Hospital (CAH)? It’s a scenario few want to imagine, but one that has surfaced repeatedly in commissioner meetings and campaign debates. Understanding what it would actually mean is essential to understanding the stakes.
The CAH designation, created in the 1990s, was meant to preserve essential healthcare in remote communities at risk of losing hospital services entirely. It offers better Medicare reimbursement—typically 101% of allowable costs—but at a steep price: hospitals must limit themselves to 25 inpatient beds, maintain specific emergency-readiness standards, and operate within narrow distance rules that prevent two CAHs from being located too close together.
That last rule alone would have serious local consequences. Because Jefferson Healthcare is already a Critical Access Hospital just 35 miles away, federal regulations would likely require OMC to close or consolidate many of its Sequim operations if it ever converted. That would mean not only reduced access for patients but also hundreds of lost jobs. Based on conversations with two hospital commissioners, Pelayo estimates the number could exceed 300 positions across the system.
While CAH status might stabilize finances on paper, it would hollow out the hospital’s capacity. OMC currently serves about 45 inpatients per day, plus thousands of outpatient visits each month. Reducing that to 25 beds would shift much of Clallam County’s medical care to Port Townsend, Kitsap, or Seattle, straining regional hospitals and forcing local families to travel long distances for routine procedures.
CAH conversion isn’t a quick fix, either—it would take years to plan, approve, and execute. In the meantime, services would likely shrink and staff uncertainty would rise. “It’s not a realistic solution in the near term,” Pelayo explains. “The better option is to stabilize what we have now and make the existing model work.”
Still, the fact that OMC has even explored CAH scenarios underscores the urgency of the moment. Financial recovery is not just about cutting losses—it’s about preserving local control before decisions are made for us.
As Pelayo summarizes, “Critical Access status might keep the lights on, but it would come at the cost of our independence, our workforce, and the level of care this community deserves.” The better path—the harder path—is to fix what’s broken while OMC still has the capacity to shape its own future.
Voices from the Community
For all the spreadsheets and dashboards, Olympic Medical Center’s story remains a human one. Every line item represents people—patients waiting for care, nurses working double shifts, or local businesses waiting to be paid. That’s what makes this crisis personal. OMC isn’t an abstract institution; it’s where our neighbors are born, healed, and comforted when they’re most vulnerable.
What’s been remarkable about this chapter is how thoughtful the community conversation has been. Across meetings, news threads, and social media discussions—many of them spurred by Pelayo’s research—citizens have managed to debate facts without falling into division. The tone has been unusually respectful for such a high-stakes issue, and that’s something worth preserving.
Healthcare workers have spoken up about the daily strain. “When bedside providers are squeezed to do more with less, patient care becomes dangerous,” one nurse wrote. Others shared frustration over staffing shortages, broken systems, and the toll of uncertainty. Pelayo agreed but added an uncomfortable truth: without a stable financial foundation, even the most dedicated teams can’t keep serving people safely. “Sustainability,” he wrote, “isn’t about putting money ahead of people—it’s about making sure we can keep caring for people for years to come.”
Community members have also weighed in on leadership. Some have questioned the cost of hiring outside consultants and an interim CEO with a national turnaround background. But as Pelayo points out, the expense is trivial compared to the $70 million OMC has already lost since 2022. “If we’d hired him two years ago, we would have lost significantly less,” he says. “His pay is irrelevant. His expertise is essential—and we need help now.”
He also notes that the interim CEO’s role is by nature temporary—and often thankless. “He’ll end up being the fall guy,” Pelayo explains. “He’s here to make the hard choices no one else wants to make, so that the next CEO can start fresh. That’s how turnarounds work.”
Still, the public tone remains one of cautious hope. Even those who disagree about tactics largely agree on one thing: OMC matters, and its survival depends on working together. “We may disagree on how to fix it,” one commenter said, “but we all want a hospital that stays open, pays its bills, and treats people with dignity.”
That spirit—rooted in realism and respect—is exactly what gives this moment potential. When a community can discuss hard truths without turning on itself, it’s already started the work of recovery.
What’s Within Our Control: A 100-Day Local Action Plan
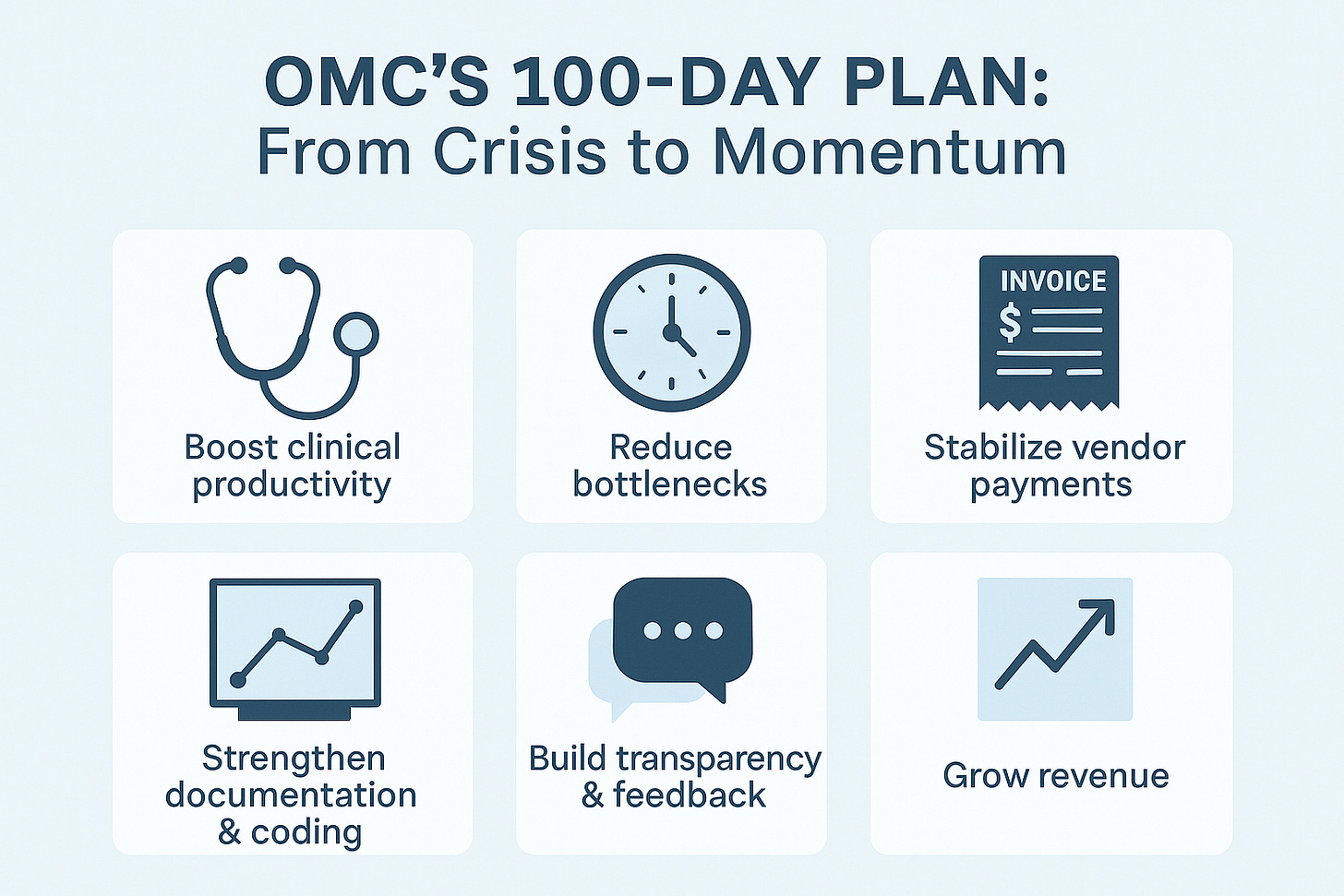
The first step in any turnaround is facing the facts; the second is acting decisively on what’s within reach. The next hundred days will determine whether Olympic Medical Center can rebuild stability and trust. As Pelayo puts it, “We have to focus on what’s within our control—and execute with urgency, consistency, and accountability.”
Drawing from Pelayo’s analysis and conversations with OMC staff and community members, the following represent his suggested areas for immediate local action—rooted in data, not politics, and focused on both stabilization and growth.
1. Increase Clinical Productivity and Access
OMC’s biggest opportunity lies in better utilization of existing staff and facilities. At recent meetings, leadership acknowledged that only a fraction of providers meet national productivity benchmarks. This isn’t about working harder; it’s about working more efficiently. By improving scheduling, closing referral loops, and expanding appointment capacity, OMC can serve more patients, reduce wait times, and capture revenue that’s currently walking out the door.
2. Reduce Service Delays and Bottlenecks
Patients across the county report months-long waits for imaging, cardiology, and orthopedic care. These aren’t staffing failures—they’re process failures. Leadership’s renewed focus on throughput metrics—like “door-to-provider time” and MRI turnaround—is key. Faster service means better outcomes, higher satisfaction, and stronger local loyalty.
3. Stabilize Vendor Payments and Rebuild Credibility
With $25–30 million owed to vendors, OMC’s relationships with local suppliers are strained. Paying those debts down in a structured, transparent way—back to the Interim CFO’s “mid-teens” target for days outstanding—will show discipline and rebuild trust. Clear communication with vendors about repayment plans is equally important.
4. Strengthen Documentation, Coding, and Revenue Capture
Revenue recovery depends on accuracy. OMC loses millions each year from documentation gaps and miscoded claims. Investing in risk adjustment and case-mix optimization training will ensure the hospital captures every dollar it’s earned. Growth doesn’t just mean more visits—it means smarter billing and fewer denials.
5. Maintain Transparency and Employee Voice
Transparency must extend beyond financial reports. OMC’s new performance dashboard should be shared publicly, even if the numbers aren’t flattering. That visibility builds credibility. Internally, employees need clear ways to provide input—an anonymous feedback system, regular town halls, and recognition for problem-solving at every level.
6. Grow Revenue, Not Just Cut Costs
OMC cannot save its way to prosperity. Sustainable recovery depends on increasing revenue through higher utilization, stronger physician retention, and expanded services. That includes rebuilding 340B eligibility, strengthening referral networks, and growing profitable outpatient care lines. “We can’t cut our way to growth,” Pelayo reminds us. “At some point, we have to grow.”
The Path Forward
These next hundred days are about momentum—visible progress that proves OMC is capable of change. None of these steps require new laws or outside bailouts. They require discipline, urgency, and steady leadership. If the hospital can demonstrate improvement—on access times, vendor payments, and utilization—confidence will begin to return.
As Pelayo says, “This isn’t about perfection; it’s about progress.” Each visible gain rebuilds trust—and each act of transparency strengthens the bridge between OMC and the community it serves.
Governance and Elections: Oversight vs. Operations
For all the attention on Olympic Medical Center’s finances, one of the most consequential decisions ahead lies outside its walls—at the ballot box. The upcoming hospital commissioner election will shape not just who governs OMC, but whether its recovery continues on course or changes direction midstream.
The question facing voters is not whether OMC needs accountability—it does—but what kind of leadership best delivers it.
The Case for Stability and Continuity
From Pelayo’s perspective, OMC’s fragile progress under Interim CEO Mark Gregson and Interim CFO Dennis Stillman depends on steady governance. “Mid-turnaround disruption,” he warns, “could stall the very progress we’ve waited years to see.”
Pelayo also points out that not all current board members share equal responsibility for past mismanagement. Penney Sanders, who joined the board in March 2025, wasn’t part of the prior leadership team that oversaw OMC’s decline. Ann Henninger, the current board chair, was involved during that period—but according to several accounts Pelayo has heard, she advocated for stronger corrective action and was outvoted by a four-member majority. That detail hasn’t been independently verified, but it may underscore a pattern of divided leadership more than deliberate neglect.
To Pelayo, the priority now is completing the turnaround already underway before shifting to long-term strategy. “Stability now,” he says, “advocacy next.” The idea is to finish implementing operational discipline before launching new initiatives or leadership changes that could slow momentum.
The Case for Fresh Perspectives
Many in the community, however, see the election as an opportunity to renew—not reset—the board. Three challengers come from healthcare backgrounds, and supporters argue that their clinical experience could make oversight more relevant to frontline realities. They see these candidates not as disruptors but as potential bridges between management and staff—leaders who can translate data into day-to-day context.
To this group, OMC’s problems are as much cultural as financial. They believe that adding commissioners with direct healthcare experience could help rebuild trust between staff and administration, ensuring that operational improvements never lose sight of patient care. “We need a board that listens to the people doing the work,” one community member wrote, “not just the people managing it.”
Finding Common Ground
These views aren’t mutually exclusive. The hospital needs both continuity and accountability, both stability and fresh insight. As Pelayo notes, the real issue isn’t incumbents versus newcomers—it’s whether commissioners understand their role: to oversee the CEO, not to manage the hospital. Good governance requires asking tough questions, respecting professional boundaries, and building trust through transparency.
Voters face a pivotal choice—but also a constructive one. Whether through continuity or renewal, OMC’s future depends on electing commissioners who value collaboration over politics, facts over rhetoric, and solutions over blame. The work ahead is too important for anything less.
Accountability, Transparency, and Follow-Through
After years of financial losses, compliance lapses, and leadership turnover, trust has become Olympic Medical Center’s most important currency. Fixing the numbers is essential—but restoring public confidence depends on what comes next: clear goals, visible results, and honest communication.
OMC’s interim leadership team has taken a major step forward by tracking and sharing performance data through its new operational dashboard. That system monitors key indicators such as cash on hand, vendor payables, provider productivity, infection rates, and patient satisfaction. The next step is making that same data available in a way the community can easily follow.
A public-facing summary, updated monthly, doesn’t need to be complicated—just consistent. The hospital could report a few key measures that matter most:
Days of cash on hand (financial stability)
Accounts payable days (timeliness of vendor payments)
Wait times for imaging and specialty care (access)
Readmission and infection rates (quality and safety)
Employee engagement or turnover (workforce health)
Tracking these same metrics over time—honestly, without spin—would demonstrate real accountability. Missed goals can be explained; hidden results can’t.
As Pelayo puts it, “Accountability isn’t a buzzword—it’s a system. It’s how you prove that talk has turned into progress.”
Clallam County Solutions will continue to monitor these measures and report on OMC’s progress in that same spirit of transparency. The goal isn’t praise or criticism—it’s clarity. Change takes time, but integrity shows up every month in the numbers.
If OMC and its board keep those commitments visible and verifiable, trust will follow—not because the community is told to believe, but because it can see the evidence for itself.
Call to Constructive Engagement
Olympic Medical Center’s story is still being written—by its staff, its leadership, and the community it serves. The numbers may look daunting, but they aren’t destiny. As Pelayo notes, this is a moment for clarity and resolve, not despair. “We can’t fix what we won’t face,” he says—and right now, OMC is finally facing it.
The outcome depends on everyone.
For staff, it means continuing to share ideas for improvement, even when change feels difficult.
For leadership, it means maintaining transparency and following through on commitments.
For commissioners, it means staying focused on oversight, not operations—and governing with discipline instead of politics.
For the community, it means engaging constructively: asking hard questions, showing up at meetings, and insisting on truth over rumor.
The challenges are real, but so are the opportunities. This turnaround isn’t just about fixing a balance sheet—it’s about preserving local healthcare that reflects who we are as a community: resilient, honest, and capable of solving problems together.
If OMC stays disciplined, transparent, and forward-looking, this crisis could become the foundation for something stronger—a hospital that not only survives but grows smarter and more sustainable for the next generation.
Because in the end, OMC’s recovery won’t be defined by what went wrong—it will be measured by what we did next.
Acknowledgment
A special thank you to Steven Pelayo for his extensive research, thoughtful analysis, and the balanced, fact-driven approach he has brought to this complex topic. His dedication to understanding both the financial and human sides of Olympic Medical Center’s challenges has been invaluable. His work—and the respectful, data-based dialogue it has inspired—formed the backbone of this article and reflects the kind of civic curiosity and constructive engagement that strengthens our community.
Glossary
340B Drug Pricing Program – A federal program allowing eligible hospitals to purchase outpatient drugs at steep discounts, often saving millions annually. OMC lost its eligibility in 2025 due to internal compliance failures, costing an estimated $8–8.5 million per year until requalification.
CAH (Critical Access Hospital) – A federal designation designed to preserve essential care in remote communities. It reimburses Medicare at 101% of allowable costs but limits hospitals to 25 inpatient beds and restricts proximity to other CAHs (Jefferson Healthcare’s status prevents OMC’s Sequim facility from qualifying).
CMS/DOH Compliance – Oversight by the Centers for Medicare & Medicaid Services and the Washington State Department of Health. Maintaining compliance is mandatory for reimbursement and continued certification.
Days of Cash on Hand – A financial measure showing how long an organization can operate using only existing cash reserves. OMC currently holds about 30 days—half the minimum required under its loan covenants.
Accounts Payable Days (AP Days) – The average number of days a hospital takes to pay its suppliers. Higher AP days signal cash-flow strain and affect vendor relationships.
wRVU (Work Relative Value Unit) – A national standard for measuring provider productivity, used to evaluate workload and compensation fairness.
UW Medicine Affiliation – A non-binding Letter of Intent signed in 2025 between OMC and UW Medicine to explore partnership structures that may strengthen specialty access and bipartisan advocacy—not a financial rescue or acquisition.
Throughput Metrics – Operational indicators of how efficiently patients move through hospital systems, such as “door-to-provider time” or imaging turnaround.
Active dialogue and engagement with our readers is crucial. Writers on this platform are encouraged—and expected—to revisit their articles regularly, responding thoughtfully to readers’ questions and concerns.
We want conversations, not shouting matches. Therefore, comments will be reviewed regularly and are expected to adhere to these foundational guidelines:
Stay on Topic: Comments must relate directly to the article.
Respectfulness: Every comment should demonstrate respect toward authors, website management, and fellow commenters. Bullying, name-calling, or disrespectful behaviors will not be tolerated.
Constructive Dialogue: Political grandstanding is unwelcome here. While some discussions naturally involve political elements, the goal is to enhance understanding, clarify perspectives, and contribute constructively.
No Personal Attacks: As Theodore Roosevelt wisely said, it’s the person who is “actually in the arena” who deserves our respect. Criticism is welcome, but personal attacks are not.
Transparency: Any new guidelines needed as this platform evolves will prioritize civility, decency, and productive dialogue.




Exceptional article. Thank you for the straightforward analysis. We are blessed to have Danny and Steven as leaders of our community that give of their time freely.
Thank you for the nuanced take.
“Even those who disagree about tactics largely agree on one thing: OMC matters, and its survival depends on working together. ‘We may disagree on how to fix it,” one commenter said, “but we all want a hospital that stays open, pays its bills, and treats people with dignity.’ That spirit—rooted in realism and respect—is exactly what gives this moment potential. When a community can discuss hard truths without turning on itself, it’s already started the work of recovery.”
With community support behind and within OMC and the turnaround underway, OMC is in the strongest position it’s had in years. Working together, we can’t fail.